An Online Eligibility Check (OEC) is generated in the same way as a standard IMC claim. The individual pages of the 'claim' dialog box are as shown here. |
|
Either a presenting illness item number, or a code is required. If there is an anaesthetic base item on the account, this will be inserted automatically.
The 'Code' field has a list of conditions/procedures generated by Medicare, one of which can be selected.
If not same day surgery, a length of stay must be provided. Admission date is also required (entered on the Operation page of the account). |
|
Details on this tab can usually be ignored. For checks involving Medicare items, the ServiceCodeTypeCode must be set to C and the other values are not required.
For fund only checks, the other fields may be used. You may need to consult with the fund to determine what is appropriate here.
Details here are set to be the same for each item. Tick the checkbox to edit item details individually (usually not required). |
|
Similar details to other Eclipse claims.
An optional email address can be provided. |
|
|
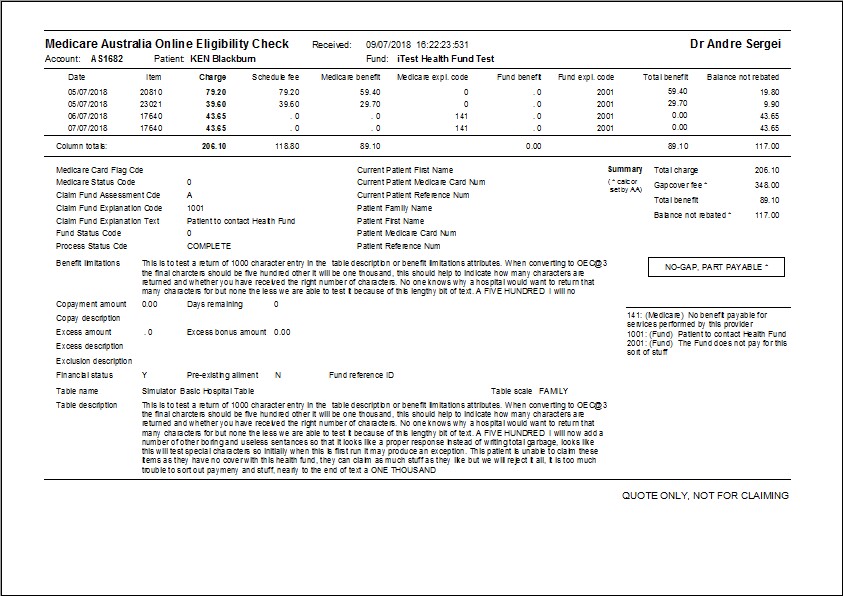
Once the OEC is transmitted, and reports retrieved, the Eclipse tab will look similar to this.
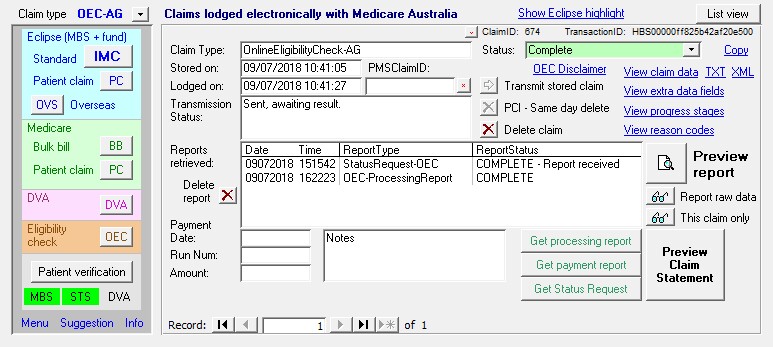
The processing report retrieved for an OEC check will look like this.