The Australian Government Department of Human Services provides a comprehensive guide to using online claiming and Eclipse. Their 'Medical and Eligibility User Guide V3.1 for Medical Practitioners' (Word doc) includes a detailed description of what you can expect with OVS and OEC functions.
Two new Eclipse functions have been added in AA version 8.9.
OVS - Overseas claiming
OEC - Online Eligibility Checking
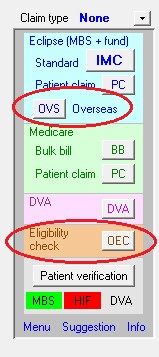
Both are available on the left side of the Eclipse tab for any account, where the other claim types are located.
Transmitting and reporting processes are essentially the same as other claim types, although there are some specific differences as noted below. |
|
Overseas Claiming (OVS)
This process sends a claim to a health fund which covers overseas patients who are not covered by Medicare. The process is essentially the same as an IMC Eclipse claim, except that there is no Medicare involvement. Claims are transmitted in the normal way, with processing reports and ERA payment reports being retrieved in the same way as for other claim types.
Notable issues are:
| • | Claims can be sent for procedures done no further than 6 months in the past. |
| • | A hospital admission date is required. |
| • | Fees vary between funds, and may be at the Medicare schedule fee only. Contact the fund for details. |
Online Eligibility Checking (OEC)
Whereas an Online Patient Verification (OPV) process checks a patient's identification and enrollment details with Medicare and their health fund, OEC checks a patient's eligibility for a specific procedure. This will take into account the level of cover the patient has with the fund, whether they are in a waiting period, and other factors that may affect their eligibility for benefits from Medicare and their fund. An eligibility check should provide confirmation of the amount that Medicare/fund will pay for a specific procedure.
Notable issues are:
| • | An eligibility check should ideally be done before a claim is sent. This requires full details of dates, items and referrals. |
| • | Some additional information is required for an eligibility check, more even than for a claim itself. |
| • | An OEC can be be done for a date 6 months into the future, but for no more than 7 days in the past. |
| • | Results of the OEC are not instantaneous. It can take up to 20 minutes to receive a response. |
| • | OEC checks are transmitted in the same way as an IMC claim, and processing reports are retrieved in the same way as IMC processing reports. |
| • | An OEC check is not a claim for payment. Depending on the result of the OEC, an IMC or other claim type may then be transmitted. |
| • | An OEC can be done for Medicare only (ECM), fund only (ECF) or Medicare and fund together (OEC). Eligibility checks do not apply to DVA patients. |
| • | For more details on sending an OEC, please click here. |
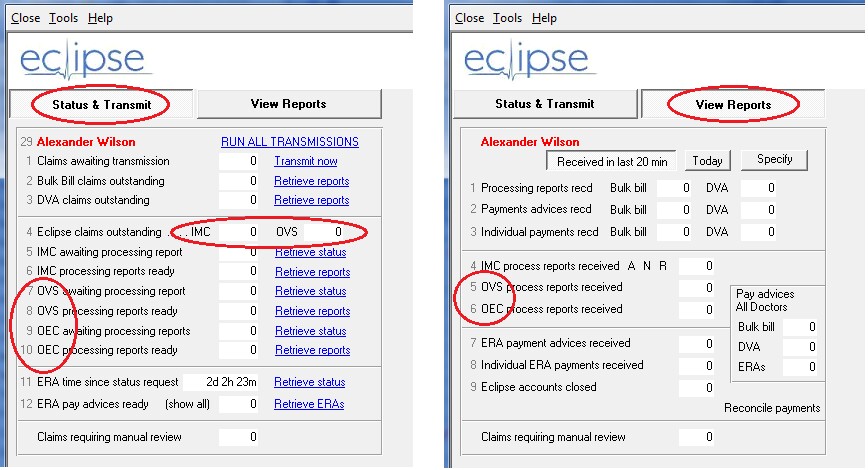
Modifications to the Eclipse Menu
The Eclipse menu has been modified to accommodate the additional elements required for the OVS and OEC processes. Rather than have all the details on one screen, the functions have been split up into two separate tabs, labeled 'Status & Transmit' and 'View Reports'. Click the relevant tab to display either the transmission or reporting details.
Notable issues are:
| • | For OVS claims, both processing reports and ERAs are available. For OEC checks, only processing reports are available. |
| • | The <Run all transmissions> process will retrieve any available OVS and OEC reports in the same way as for other reports. |
| • | Clients may wish to retrieve eligibility check reports more frequently that other report types. This can be done individually using the <Retrieve status> or <Retrieve reports> button in rows 9 and 10. Like other report types, it is necessary to retrieve the status of the reports before retrieving the reports themselves. |
| • | Status and processing reports for OVS and OEC can also be retrieved from the Eclipse tab of any individual account. |